While most types of this virus are harmless and practically undetectable, genital HPV can be a high-risk infection and the main culprit of most cervical and anal cancer cases.
In fact, it’s estimated that about 46,100 HPV-related cancers occur each year in the United States, with both men and women being at risk.
In this article, we’ll guide you through the most common symptoms of HPV, discuss how it is transmitted, whether it’s preventable, and help you understand possible treatment options and the importance of early detection.
What is HPV?
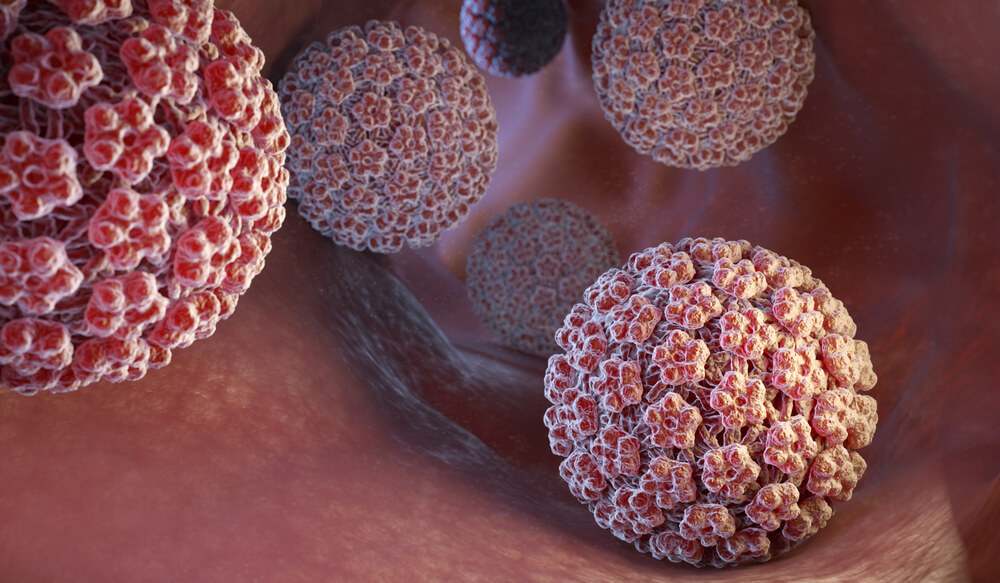
Human papillomavirus (HPV) is a widely common virus that doesn’t pose a threat in most cases. With more than 150 known types, exposure to HPV is almost unavoidable. It essentially affects the skin but can only live in cells called squamous epithelial cells (mostly found on mucosal skin surfaces). HPV will thus usually affect:
- Vaginal cannal, cervix, and vulva
- Anal and rectal mucosa
- Penile foreskin and scrotum
- The mucous membrane of the nose, mouth, and throat
- The trachea and bronchi
Most infections go away on their own in the span of two years without any notable symptoms or health complications. However, sexually-transmitted HPV can manifest in the form of genital warts (papillomas) or cause abnormal cell mutations that can lead to cancer.
How is HPV transmitted, and is it common?
In 2018 it was estimated that a whopping 45.2 million Americans in the US were infected with HPV, and each year 14 million new infections occur. Essentially, since it’s very common and spreads quickly, most men and women will get a benign HPV infection in their lifetime.
HPV is not transmitted through bodily fluids and blood but rather through direct skin-to-skin contact.
Contrary to popular belief, penetrative sex is not the only way of transmission. In fact, any type of genital skin contact with an HPV infected person (including oral or anal sex or sharing sex toys or intimate items) could be enough to catch the virus, even if the person isn’t experiencing any symptoms.
A common myth is that only individuals who have had many sexual partners are prone to STIs, but the truth is that even people who are sexually active for the first time are just as exposed to HPV as others.
HPV symptoms in men
Men do get infected with HPV; however, they most often don’t express any noticeable symptoms. Infected men won’t show any specific telltale signs of this STI. High-risk HPV types can cause visible genital and anal warts that often go unnoticed by health practitioners.
Since there’s no standardized treatment for asymptomatic HPV, most infections in men pass by on their own, but there is still a significant risk of transmission.
Men are not safe from potential anal or penile cancer induced by this virus. Therefore regular checkups and prevention are necessary for a positive outcome.
HPV and women: symptoms and risks
HPV symptoms in women will depend on the type of HPV infection.
Some low-risk HPV types can cause genital or cervical warts. These skin protrusions usually appear as flesh-colored, raised, or flat bumps that are sometimes even prone to bleeding, so they’re often misinterpreted as menstrual spotting. Genital warts can occur months after the infection contact and can sometimes get disregarded since there are no other indications of the virus that would call for testing.
On the other hand, high-risk HPV types usually don’t manifest in symptoms at all but can cause changes to the cells in the cervix, vulva, and anus, leading to cancer. All cases of cervical cancer are caused by HPV. However, not all women who are HPV positive will develop cancer. Regular monitoring of high-risk HPV infections can significantly lower the chances of getting cancer.
Advanced cervical and vaginal cancer, however, may be related to symptoms such as:
- Uncommon bleeding after sex or unrelated to the cycle
- Unusual vaginal HPV discharge
- Sharp pelvic pain
- Pain during intercourse
- Urinary discomfort and bleeding
- Extreme weight loss
Testing and diagnosing: How do I know I have HPV?
Since they don’t develop into cancer, low-risk HPV infections are usually diagnosed by examining genital warts, so no testing is needed. Men are not subjected to HPV testing. In fact, there is no FDA-approved test for HPV in men since they usually recover without any significant health consequences.
Due to the increasing concerns about cervical cancer development, testing for high-risk HPV in women has become a standardized practice and is highly recommended.
The first stage in detecting HPV is regular Pap testing which should be done at least once a year as a part of regular gynecologist checkups. A Pap smear doesn’t test for HPV but instead checks if there are any cell abnormalities in the cervix. Healthy women under 30 are not routinely subjected to HPV testing. However, your OB-GYN may perform an HPV test if your Pap smear shows irregularities. In that case, reliable facilities, such as STD testing in Miami, Florida, will perform a routine HPV test by collecting cervix cells to check for the virus.
Furthermore, women over 30, especially in their 40s, are at a higher risk of cervical cancer, so co-testing (both pap test and HPV test) may be a part of your examination.
Detecting high-risk HPV is crucial for managing precancerous and early-stage cancer cases, opening a chance for encouraging and promising prognosis in the future.

HPV prevention: Can I protect myself from HPV?
The nature of HPV quick-spreading still makes it a highly transmissive disease, and you can’t fully protect yourself from it.
That said, there are ways you can increase your chances of staying healthy.
Avoid any contact with an HPV-positive person that includes the areas that could be infected, such as the mouth, anus, and vaginal area.
Using condoms during intercourse may help by significantly lowering the risk of an HPV infection, but it still isn’t 100% effective.
Limiting the number of sexual partners will not make you immune to HPV, but it may lower the chances of getting in contact with an infected person.
HPV vaccines are a reliable preventative measure designed to protect from genital warts and cancer-inducing HPV types but are only effective when given at an early age (usually 9-12 year-olds). Depending on your region or country, HPV vaccine administration regulations will differ.
Finally, doing regular OB-GYN checkups and Pap tests to stay on the safe side is the most reliable method of HPV-related cancer prevention. Finding a trustworthy specialist like the ones at Obstetrics and Gynecology In South Miami is essential for developing a healthy and responsible approach to regular testing and opening the opportunity for early disease detection.


