Menopause marks a significant phase in a woman’s life, accompanied by various changes in the body. One aspect often overlooked is its impact on bone health. As estrogen levels decline, bone density may decrease, leading to conditions like osteoporosis. In this article, find out more about the intricate relationship between menopause and bone health, exploring why does menopause cause osteoporosis, how to prevent osteoporosis after menopause and what steps can be taken to mitigate the condition.
Obstetrics and Gynecology In South Miami, Florida stands out as the premier choice for women’s healthcare for several compelling reasons. Firstly, the practice boasts a team of highly skilled and experienced obstetricians and gynecologists who are dedicated to providing personalized and compassionate care to each patient. Their expertise covers a wide range of women’s health issues, from routine gynecological exams to complex obstetric procedures, ensuring comprehensive and specialized care at every stage of a woman’s life.
The Connection Between Menopause and Bone Health
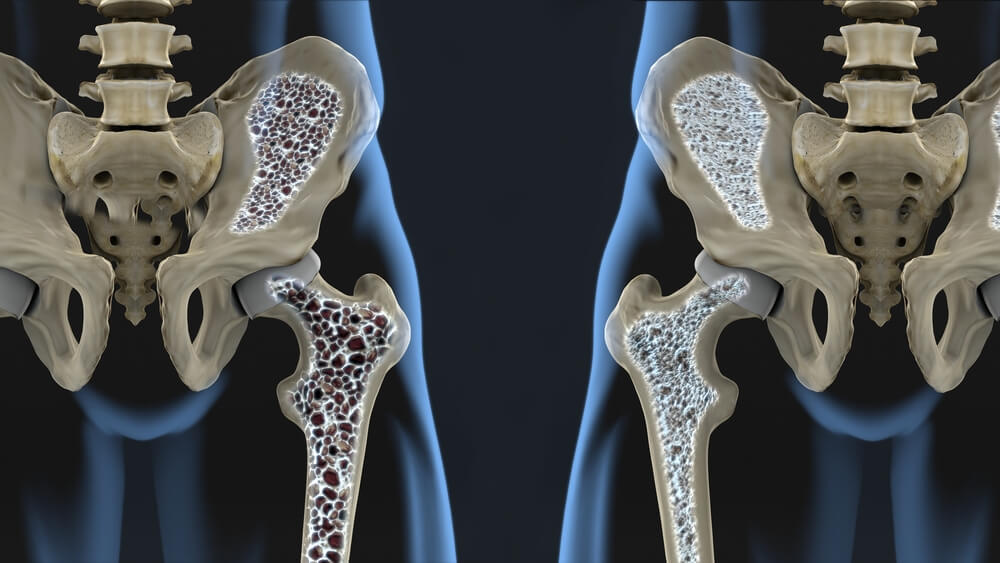
The connection between menopause and bone health is rooted in the hormonal changes that accompany this natural transition in a woman’s life. During menopause, estrogen levels decline significantly, disrupting the delicate balance between bone formation and resorption. Estrogen plays a crucial role in maintaining bone density by inhibiting bone breakdown, or resorption, while also stimulating the activity of bone-forming cells called osteoblasts.
With lower estrogen levels, bone turnover accelerates, leading to a net loss of bone mass and density. This phenomenon, known as “menopause bone loss,” increases the risk of osteoporosis, a condition characterized by brittle and fragile bones prone to fractures. Consequently, menopausal women are particularly vulnerable to osteoporosis, emphasizing the importance of proactive measures to preserve bone health during this critical phase of life.
Osteoporosis and Menopause
Osteoporosis and menopause share a close and often consequential relationship, with the hormonal changes of menopause significantly impacting bone health. As estrogen levels decline during menopause, the body’s ability to maintain bone density becomes compromised. As mentioned, estrogen plays a crucial role in regulating bone turnover, inhibiting bone resorption while promoting bone formation.
Without adequate estrogen, bone resorption outpaces formation, leading to a gradual loss of bone density and strength i.e. the menopause bone loss. This increased bone fragility raises the risk of osteoporosis, a condition characterized by weakened bones susceptible to fractures. As such, proactive measures to preserve bone health, such as adequate nutrition, weight-bearing exercises, and medical interventions, are vital for women navigating the menopausal transition.
Why Does Menopause Cause Osteoporosis?
Several mechanisms contribute to the development of osteoporosis during menopause. Firstly, estrogen as explained above plays a pivotal role in maintaining osteoblast activity, the cells responsible for bone formation. Secondly, estrogen deficiency enhances osteoclast activity, the cells responsible for bone resorption, resulting in accelerated bone loss. Moreover, menopause coincides with age-related declines in bone density, amplifying the impact of hormonal changes.
Menopausal Osteoporosis
Menopausal osteoporosis refers to osteoporosis that occurs as a result of menopause-related hormonal changes. It is characterized by rapid bone loss and an increased risk of fractures, particularly in weight-bearing bones such as the spine, hips, and wrists. Women experiencing early menopause or those with surgical menopause (removal of ovaries) are at even greater risk. Menopausal osteoporosis underscores the importance of proactive measures to preserve bone health during this critical phase of life.
How to Prevent Osteoporosis After Menopause?
While menopause may accelerate bone loss, proactive steps can help mitigate its impact and reduce the risk of osteoporosis. Here are some strategies to safeguard bone health:
Balanced Diet: A balanced diet is essential for maintaining overall health and well-being. It involves consuming a variety of nutrient-rich foods from all food groups, including fruits, vegetables, whole grains, lean proteins, and healthy fats. By incorporating a diverse range of foods into your meals, you can ensure that your body receives the necessary vitamins, minerals, and other essential nutrients it needs to function optimally.
A balanced diet not only provides energy for daily activities but also supports proper growth, development, and immune function. Moreover, it can help prevent chronic diseases such as obesity, diabetes, and heart disease when combined with regular physical activity and healthy lifestyle habits.
Regular Exercise: Regular exercise is a cornerstone of a healthy lifestyle, offering numerous physical and mental benefits. Engaging in physical activity on a consistent basis helps strengthen muscles, improve cardiovascular health, and enhance flexibility and endurance. It also plays a crucial role in weight management by burning calories and promoting fat loss.
Beyond its physical benefits, regular exercise is linked to improved mood and reduced stress levels, thanks to the release of endorphins, the body’s natural mood elevators. Incorporating various forms of exercise into your routine, such as aerobic activities, strength training, and flexibility exercises, can maximize the overall health benefits and contribute to a higher quality of life.
Lifestyle Modifications: Lifestyle modifications encompass a wide range of changes aimed at improving overall health and well-being. These adjustments may include quitting smoking, reducing alcohol consumption, improving sleep habits, managing stress effectively, and maintaining a healthy weight. Making these changes can significantly reduce the risk of developing chronic diseases such as heart disease, diabetes, and certain cancers.
By adopting a healthier lifestyle, individuals can experience increased energy levels, improved mood, and enhanced cognitive function. Moreover, these modifications contribute to a greater sense of overall satisfaction and fulfillment in life.
Bone Density Testing: Bone density testing, also known as dual-energy X-ray absorptiometry (DEXA), is a non-invasive diagnostic procedure used to assess bone health and detect osteoporosis. During the test, specialized X-ray equipment measures bone mineral density (BMD) at various sites, typically the spine, hip, or wrist. The results provide valuable information about bone strength and fracture risk, helping healthcare providers diagnose osteoporosis and monitor its progression.
Bone density testing is recommended for postmenopausal women, individuals with risk factors for osteoporosis, and those undergoing long-term treatment with medications that may affect bone health. Early detection through bone density testing allows for timely intervention and the implementation of strategies to prevent fractures and maintain bone health.
Hormone Replacement Therapy (HRT): Hormone Replacement Therapy (HRT) involves the administration of estrogen and, in some cases, progesterone to alleviate symptoms of menopause and prevent osteoporosis in postmenopausal women. It aims to replenish declining hormone levels, particularly estrogen, which can help alleviate hot flashes, night sweats, vaginal dryness, and mood swings.
HRT can also help maintain bone density and reduce the risk of fractures associated with osteoporosis. However, it is important to weigh the benefits against potential risks, including an increased risk of blood clots, stroke, breast cancer, and cardiovascular disease. Therefore, it is crucial for women to discuss the risks and benefits of HRT with their healthcare provider to make an informed decision tailored to their individual health needs.
Conclusion
Menopause heralds a new chapter in a woman’s life, accompanied by various physiological changes, including alterations in bone health. The decline in estrogen levels during menopause can predispose women to osteoporosis, a condition characterized by fragile bones and increased fracture risk.
However, with awareness and proactive measures, women can safeguard their bone health and mitigate the effects of menopausal bone loss. Having a balanced lifestyle, incorporating exercise, and seeking appropriate medical guidance, women can navigate this transition with resilience and maintain strong, healthy bones well into their golden years. Our medical center is there for you for any questions or concerns, so feel free to contact us.


