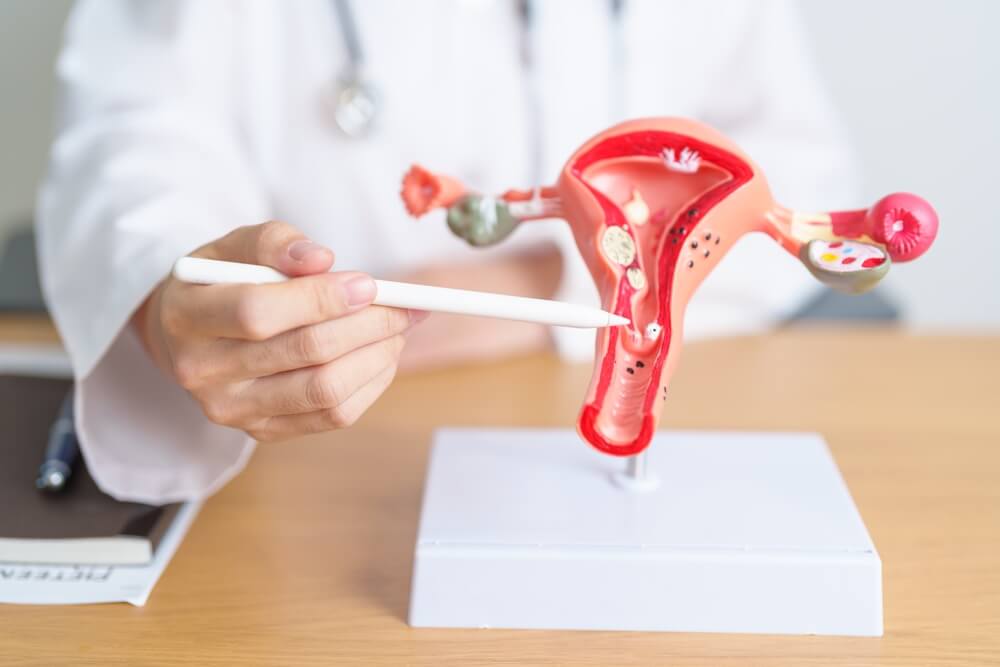
When an ectopic pregnancy develops, the pregnancy takes place outside of the uterus. This can happen when the fertilized egg accidentally implants in a place where fetal growth isn’t supported. These places will often include the fallopian tube and early in one of the ovaries, the cervix, or the abdominal cavity.
All trained pregnancy specialists, such as Dr. Jessica White, are well aware of the severity of these cases. These pregnancies can’t continue because the uterus is the only organ capable of carrying out a pregnancy. That said, these pregnancies can become potentially life-threatening.
In this article, we’ll discuss the essentials you need to know about ectopic pregnancies and the most common symptoms and treatment options. Still, the focal point of this article is how to diagnose an ectopic pregnancy and whether they can show up on pregnancy tests.
Causes and Symptoms
First of all, we need to say that these pregnancies are quite rare, occurring only around 2% of all pregnancies.
In most cases, the factors leading to ectopic pregnancies are conditions that block or slow the egg’s movement along the fallopian tube.
These factors may be the following:
- The presence of adhesions, scar tissue, or inflammation due to pelvic surgery.
- Damage in the fallopian tubes due to sexually transmitted diseases.
- Being born with an irregularly-shaped fallopian tube
- A growth is blocking the egg’s path in the tube.
The early symptoms of the conditions are incredibly similar to that of standard pregnancy symptoms, but women with ectopic pregnancies may also experience additional problems, including the following:
- Vaginal bleeding
- Pain in the pelvis, lower abdomen, and lower back
- Weakness and dizziness
If the problem worsens to the point that the fallopian tube ruptures, it could lead to severe bleeding, which may also produce the following symptoms:
- Hypotension or low blood pressure
- Fainting
- Shoulder pain
- Rectal pressure
When the fallopian tube bursts, women may also feel a sharp and sudden pain in the lower abdomen. Naturally, this is a medical emergency that needs to be addressed immediately.
Risk Factors
There may be several risk factors that can increase the chances of developing such a pregnancy. They are the following:
- A history of PID or pelvic inflammatory disease and inflammation may lead to scar tissue formation.
- Previous ectopic pregnancy.
- A history of infertility.
- A history of smoking.
- A history of STDs.
- Endometriosis.
- Infertility treatments such as IVF (in vitro fertilization).
- Having an IUD at the time of conception.
- Prior surgery to the fallopian tubes or other organs in the area of the pelvis.
- Age: women over 35 have a higher risk.
Complications
An ectopic pregnancy is a severe condition (a medical emergency), as the uterus is the only organ that’s able to cater to the needs of the growing fetus. The organ can expand and stretch as the fetus develops. On the other hand, the fallopian tubes aren’t flexible enough and will burst as the fertilized egg starts to grow. The rupture can lead to profuse, life-threatening internal bleeding. As such, an ectopic pregnancy needs to be addressed immediately to avoid an injury to the fallopian tubes and the other organs. On the other hand, immediate treatment will also avoid bleeding and, as such, fatal consequences.
How To Diagnose an Ectopic Pregnancy?
Now that you understand the severity of the condition, we’ll discuss the diagnostic process.
Does an Ectopic pregnancy show up on a pregnancy test? Several women who are concerned about ectopic pregnancy may wonder about this. In short, yes, you can have a positive ectopic pregnancy test, as these conditions will still produce human growth hormones, which the test will handle as a positive pregnancy test. Furthermore, women with ectopic pregnancies will also experience some of the earliest pregnancy symptoms, like spotting, nausea, sore breasts, etc. The more concerning symptoms of an ectopic pregnancy, like abdominal pain and bleeding, will appear a bit later, somewhere around six to eight weeks.
As said above, positive ectopic pregnancy tests do not differ from standard tests, and as such, most women aren’t even aware of the fact that they have an ectopic pregnancy until they have their first prenatal appointment.
If your provider suspects the presence of an ectopic pregnancy, they may recommend several tests and examinations to establish a proper diagnosis.
Apart from a routine pelvic exam, these tests may be the following:
- Urine test: This examination involves either urinating on a test strip or providing a urine sample in a cup at your healthcare provider’s office. Subsequently, a test strip is dipped into the urine sample to obtain results.
- Blood test: Your healthcare provider may conduct a blood test to determine the human chorionic gonadotropin (HCG) hormone level in your body. HCG is only produced during pregnancy. A low level of HCG may indicate an ectopic pregnancy since HCG levels typically rise significantly when a fertilized egg implants in the uterus.
- Ultrasound examination: An ultrasound employs sound waves to generate an image of the internal structures within your body. Your healthcare provider will use this test to locate the site of implantation of the fertilized egg.
If the provider thinks the fallopian tubes have ruptured, they may also perform culdocentesis, but only in rare cases.
After the provider establishes a positive diagnosis, they will discuss the most effective treatment options with the patient. Typically, these pregnancies are discovered early, usually within the first trimester, generally around the eighth week.
Treatment
So, can an ectopic pregnancy be detected by a pregnancy test? Yes, and no. The test will register it as positive, just like it would do with a healthy pregnancy. Still, the ectopic nature of the pregnancy can only be properly diagnosed by trained experts. Furthermore, they are the best-certified professionals to recommend treatment as well.
On that note, providers may recommend surgery or medication to address to condition.
Medication for Treating Ectopic Pregnancy
There are cases when providers may suggest using methotrexate, a compound capable of stopping the fertilized egg from developing further. This medication should cause no damage to the fallopian tubes. However, it can’t be used if the tube has already ruptured.
Typically, the compound is administered as a simple injection, but it will still require follow-up appointments to monitor the patient’s HCG (human growth hormone) levels. This is crucial because, in rare cases, a second injection of the compound may be necessary if the levels of HCG remain elevated in the patient.

Surgery
If your fallopian tube has ruptured or there is a risk of rupture, your healthcare provider will recommend surgical removal of the ectopic pregnancy. This is considered an emergency surgery and is a critical and life-saving treatment. Typically, the procedure is performed laparoscopically while under anesthesia, using several small incisions in your abdomen. During the surgery, the surgeon may either remove the entire fallopian tube with the fertilized egg still inside it or remove the egg from the tube while preserving the fallopian tube.
In both cases, treatment will be fatal for the fetus, and the pregnancy will be lost.
Plan Ahead
While pregnancy isn’t always possible to plan, if you and your partner are thinking about conceiving, the best and safest option is to schedule an appointment with your prenatal care specialist. This will ensure that your journey will start off the right way, with every concern and question answered from the start.
That said, feel free to schedule an appointment at our practice today.


